Normal Values: Difference between revisions
Jump to navigation
Jump to search
m (→References) |
|||
| (51 intermediate revisions by 5 users not shown) | |||
| Line 1: | Line 1: | ||
=Left Ventricle= | Below an up-to-date list of echocardiographic normal values. | ||
=Left Ventricle= | |||
==Left Ventricular Systolic Function== | |||
{| class="wikitable" style="font-size:90%;" | |||
|+'''Reference limits and values and partition values of left ventricular function<cite>ASE</cite>''' | |||
|- | |||
! rowspan="2" style="width:200px" | | |||
! colspan="4" | Women !! colspan="4" | Men | |||
|- | |||
! style="width:80px" | Reference range | |||
! style="width:80px" | Mildly abnormal | |||
! style="width:80px" | Moderately abnormal | |||
! style="width:80px" | Severely abnormal | |||
! style="width:80px" | Reference range | |||
! style="width:80px" | Mildly abnormal | |||
! style="width:80px" | Moderately abnormal | |||
! style="width:80px" | Severely abnormal | |||
|- | |||
| colspan="9" | '''Linear method''' | |||
|- | |||
| style="padding-left:12px" | Endocardial fractional shortening, % | |||
| align="center" | 27–45 | |||
| align="center" | 22–26 | |||
| align="center" | 17–21 | |||
| align="center" | ≤16 | |||
| align="center" | 25–43 | |||
| align="center" | 20–24 | |||
| align="center" | 15–19 | |||
| align="center" | ≤14 | |||
|- | |||
| style="padding-left:12px" | Midwall fractional shortening, % | |||
| align="center" | 15–23 | |||
| align="center" | 13–14 | |||
| align="center" | 11–12 | |||
| align="center" | ≤10 | |||
| align="center" | 14–22 | |||
| align="center" | 12–13 | |||
| align="center" | 10–11 | |||
| align="center" | ≤10 | |||
|- | |||
| colspan="9" | '''2D Method''' | |||
|- | |||
| style="padding-left:12px" |<font color="green">''' Ejection fraction, %'''</font> | |||
| align="center" |<font color="green">''' ≥55'''</font> | |||
| align="center" | <font color="green">'''45–54'''</font> | |||
| align="center" |<font color="green">''' 30–44'''</font> | |||
| align="center" |<font color="green">''' <30'''</font> | |||
| align="center" | <font color="green">'''≥55'''</font> | |||
| align="center" |<font color="green">''' 45–54'''</font> | |||
| align="center" | <font color="green">'''30–44'''</font> | |||
| align="center" | <font color="green">'''<30'''</font> | |||
|- | |||
| colspan="9" | <ul> | |||
<li>2D, Two-dimensional.</li> | |||
<li><font color="green">'''Green values'''</font>: Recommended and best validated.</li> | |||
</ul> | |||
|} | |||
==Left Ventricular Diastolic Function== | |||
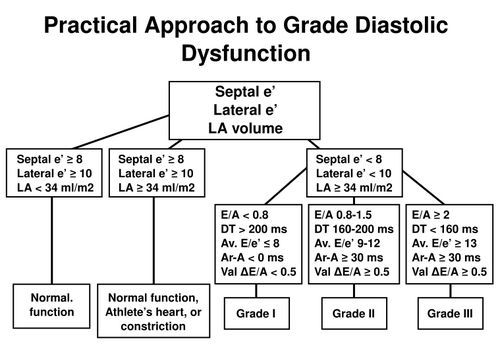
[[File:diastolicfunction.svg|500px|thumb|left|Practical approach to LV diastolic function grading. Ater <cite>ASEDF</cite>]] | |||
{{clr}} | |||
{| class="wikitable" style="font-size:90%;" | |||
|+'''Normal values for Doppler-derived diastolic measurements<cite>ASEDF</cite>''' | |||
|- | |||
! style="border-bottom:hidden" | | |||
! colspan="4" | Age group (y) | |||
|- | |||
! style="width:120px" | Measurement | |||
! 16-20 | |||
! 21-40 | |||
! 41-60 | |||
! >60 | |||
|- | |||
| IVRT (ms) | |||
| align="center" | 50 ± 9 (32-68) | |||
| align="center" | 67 ± 8 (51-83) | |||
| align="center" | 74 ± 7 (60-88) | |||
| align="center" | 87 ± 7 (73-101) | |||
|- | |||
| E/A ratio | |||
| align="center" | 1.88 ± 0.45 (0.98-2.78) | |||
| align="center" | 1.53 ± 0.40 (0.73-2.33) | |||
| align="center" | 1.28 ± 0.25 (0.78-1.78) | |||
| align="center" | 0.96 ± 0.18 (0.6-1.32) | |||
|- | |||
| DT (ms) | |||
| align="center" | 142 ± 19 (104-180) | |||
| align="center" | 166 ± 14 (138-194) | |||
| align="center" | 181 ± 19 (143-219) | |||
| align="center" | 200 ± 29 (142-258) | |||
|- | |||
| A duration (ms) | |||
| align="center" | 113 ± 17 (79-147) | |||
| align="center" | 127 ± 13 (101-153) | |||
| align="center" | 133 ± 13 (107-159) | |||
| align="center" | 138 ± 19 (100-176) | |||
|- | |||
| PV S/D ratio | |||
| align="center" | 0.82 ± 0.18 (0.46-1.18) | |||
| align="center" | 0.98 ± 0.32 (0.34-1.62) | |||
| align="center" | 1.21 ± 0.2 (0.81-1.61) | |||
| align="center" | 1.39 ± 0.47 (0.45-2.33) | |||
|- | |||
| PV Ar (cm/s) | |||
| align="center" | 16 ± 10 (1-36) | |||
| align="center" | 21 ± 8 (5-37) | |||
| align="center" | 23 ± 3 (17-29) | |||
| align="center" | 25 ± 9 (11-39) | |||
|- | |||
| PV Ar duration (ms) | |||
| align="center" | 66 ± 39 (1-144) | |||
| align="center" | 96 ± 33 (30-162) | |||
| align="center" | 112 ± 15 (82-142) | |||
| align="center" | 113 ± 30 (53-173) | |||
|- | |||
| Septal e´ (cm/s) | |||
| align="center" | 14.9 ± 2.4 (10.1-19.7) | |||
| align="center" | 15.5 ± 2.7 (10.1-20.9) | |||
| align="center" | 12.2 ± 2.3 (7.6-16.8) | |||
| align="center" | 10.4 ± 2.1 (6.2-14.6) | |||
|- | |||
| Septal e´/a´ ratio | |||
| align="center" | 2.4<sup>∗</sup> | |||
| align="center" | 1.6 ± 0.5 (0.6-2.6) | |||
| align="center" | 1.1 ± 0.3 (0.5-1.7) | |||
| align="center" | 0.85 ± 0.2 (0.45-1.25) | |||
|- | |||
| Lateral e´ (cm/s) | |||
| align="center" | 20.6 ± 3.8 (13-28.2) | |||
| align="center" | 19.8 ± 2.9 (14-25.6) | |||
| align="center" | 16.1 ± 2.3 (11.5-20.7) | |||
| align="center" | 12.9 ± 3.5 (5.9-19.9) | |||
|- | |||
| Lateral e´/a´ ratio | |||
| align="center" | 3.1<sup>∗</sup> | |||
| align="center" | 1.9 ± 0.6 (0.7-3.1) | |||
| align="center" | 1.5 ± 0.5 (0.5-2.5) | |||
| align="center" | 0.9 ± 0.4 (0.1-1.7) | |||
|- | |||
| colspan="5" | <ul> | |||
<li>Data are expressed as mean ± SD (95% confidence interval). Note that for e´ velocity in subjects aged 16 to 20 years, values overlap with those for subjects aged 21 to 40 years. This is because e´ increases progressively with age in children and adolescents. Therefore, the e´ velocity is higher in a normal 20-year-old than in a normal 16-year-old, which results in a somewhat lower average e´ value when subjects aged 16 to 20 years are considered.</li> | |||
<li><sup>∗</sup> Standard deviations are not included because these data were computed, not directly provided in the original articles from which they were derived.</li> | |||
</ul> | |||
|} | |||
==Left Ventricular Mass and Geometry== | ==Left Ventricular Mass and Geometry== | ||
{| class="wikitable" style="font-size:90%;" | {| class="wikitable" style="font-size:90%;" | ||
| Line 231: | Line 400: | ||
|} | |} | ||
=Right Ventricle= | =Right Ventricle= | ||
==Right Ventricular and Pulmonary Artery Size== | ==Right Ventricular and Pulmonary Artery Size== | ||
| Line 398: | Line 502: | ||
|- | |- | ||
| colspan=" | | TAPSE, (cm) | ||
| align="center" | 1.5-2.0<cite>ASE</cite> | |||
| align="center" | 1.3-1.5<cite>Hamer</cite> | |||
| align="center" | 1.0-1.2<cite>Hamer</cite> | |||
| align="center" | <1.0<cite>Hamer</cite> | |||
|- | |||
| colspan="6" | | |||
<ul> | <ul> | ||
<li>RV, Right ventricular.</li> | <li>RV, Right ventricular.</li> | ||
| Line 405: | Line 516: | ||
|} | |} | ||
=Atria= | =Atria= | ||
==Left Atrial Dimensions / Volumes== | ==Left Atrial Dimensions / Volumes== | ||
| Line 519: | Line 631: | ||
|} | |} | ||
==Left Atrial Pressure== | |||
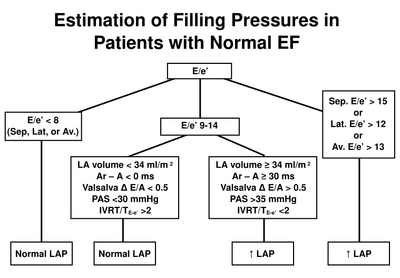
[[File:LAP_normalEF.svg|thumb|left|400px|Estimation of left atrial pressure in normal LVEF. After <cite>ASEDF</cite>]] | |||
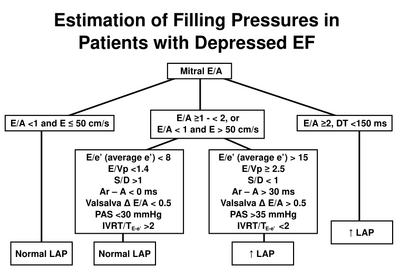
[[File:LAP_reducedEF.svg|thumb|400px|Estimation of left atrial pressure in reduced LVEF. After <cite>ASEDF</cite>]] | |||
{{clr}} | |||
=Aortic Valve= | =Aortic Valve= | ||
| Line 524: | Line 640: | ||
{| class="wikitable" style="font-size:90%;" | {| class="wikitable" style="font-size:90%;" | ||
|+'''Recommendations for classification of AS severity''' | |+'''Recommendations for classification of AS severity<cite>ASEVS</cite>''' | ||
|- | |- | ||
| Line 570: | Line 686: | ||
|- | |- | ||
| colspan="5" |<ul> | | colspan="5" |<ul> | ||
<li><sup>a</sup>ESC Guidelines.</li> | <li><sup>a</sup>ESC Guidelines.<cite>ESCAS</cite></li> | ||
<li><sup>b</sup>AHA/ACC Guidelines.</li> | <li><sup>b</sup>AHA/ACC Guidelines.<cite>AHAAS</cite></li> | ||
</ul> | </ul> | ||
|} | |} | ||
==Aortic regurgitation - severity== | |||
{| class="wikitable" style="font-size:90%;" | |||
|+'''Application of specific and supportive signs, and quantitative parameters in the grading of aortic regurgitation severity<cite>ASERE</cite>''' | |||
|- | |||
! style="width:160px" | | |||
! style="width:250px" | Mild | |||
! colspan="2" | Moderate | |||
! style="width:250px" | Severe | |||
|- | |||
! Specific signs for AR severity | |||
| style="vertical-align:top" | <ul> | |||
<li>Central Jet, width < 25% of LVOT<sup>ς</sup></li> | |||
<li>Vena contracta < 0.3 cm<sup>ς</sup></li> | |||
<li>No or brief early diastolic flow reversal in descending aorta</li> | |||
</ul> | |||
| style="vertical-align:top" colspan="2" | <ul><li>Signs of AR>mild present but no criteria for severe AR</li></ul> | |||
| style="vertical-align:top" | <ul> | |||
<li>Central Jet, width ≥ 65% of LVOT<sup>ς</sup></li> | |||
<li>Vena contracta > 0.6cm<sup>ς</sup></li> | |||
</ul> | |||
|- | |||
! Supportive signs | |||
| style="vertical-align:top" | <ul> | |||
<li>Pressure half-time > 500 ms</li> | |||
<li>Normal LV size<sup>∗</sup></li> | |||
</ul> | |||
| style="vertical-align:top" colspan="2" | <ul><li>Intermediate values</li></ul> | |||
| <ul> | |||
<li>Pressure half-time < 200 ms</li> | |||
<li>Holodiastolic aortic flow reversal in descending aorta</li> | |||
<li>Moderate or greater LV enlargement<sup>∗∗</sup></li> | |||
</ul> | |||
|- | |||
| colspan="5" | '''Quantitative parameters<sup>ψ</sup>''' | |||
|- | |||
| style="padding-left:12px" | R Vol, ml/beat | |||
| align="center" | < 30 | |||
| align="center" style="width:125px" | 30-44 | |||
| align="center" style="width:125px" | 45-59 | |||
| align="center" | ≥ 60 | |||
|- | |||
| style="padding-left:12px" | RF % | |||
| align="center" | < 30 | |||
| align="center" | 30-39 | |||
| align="center" | 40-49 | |||
| align="center" | ≥ 50 | |||
|- | |||
| style="padding-left:12px" | EROA, cm<sup>2</sup> | |||
| align="center" | < 0.10 | |||
| align="center" | 0.10-0.19 | |||
| align="center" | 0.20-0.29 | |||
| align="center" | ≥ 0.30 | |||
|- | |||
| colspan="5" | | |||
<ul> | |||
<li><em>AR</em>, Aortic regurgitation; <em>EROA</em>, effective regurgitant orifice area; <em>LV</em>, left ventricle; <em>LVOT</em>, left ventricular outflow tract; <em>R Vol</em>, regurgitant volume; <em>RF</em>, regurgitant fraction.</li> | |||
<li><sup>∗</sup> LV size applied only to chronic lesions. Normal 2D measurements: LV minor-axis ≤ 2.8 cm/m<sup>2</sup>, LV end-diastolic volume ≤ 82 ml/m<sup>2</sup> (2).</li> | |||
<li><sup>ς</sup> At a Nyquist limit of 50–60 cm/s.</li> | |||
<li><sup>∗∗</sup> In the absence of other etiologies of LV dilatation.</li> | |||
<li><sup>ψ</sup> Quantitative parameters can help sub-classify the moderate regurgitation group into mild-to-moderate and moderate-to-severe regurgitation as shown.</li> | |||
</ul> | |||
|} | |||
=Mitral Valve= | |||
==Mitral regurgitation - severity== | |||
{| class="wikitable" style="font-size:90%;" | |||
|+'''Application of specific and supportive signs, and quantitative parameters in the grading of mitral regurgitation severity<cite>ASERE</cite>''' | |||
|- | |||
! style="width:160px" | | |||
! style="width:250px" | Mild | |||
! colspan="2" | Moderate | |||
! style="width:250px" | Severe | |||
|- | |||
! Specific signs of severity | |||
| style="vertical-align:top" | <ul> | |||
<li>Small central jet <4 cm<sup>2</sup> or <20% of LA area<sup>ψ</sup></li> | |||
<li>Vena contracta width <0.3 cm</li> | |||
<li>No or minimal flow convergence</li> | |||
</ul> | |||
| style="vertical-align:top" colspan="2" | <ul><li>Signs of MR>mild present, but no criteria for severe MR</li></ul> | |||
| style="vertical-align:top" | <ul> | |||
<li>Vena contracta width ≥ 0.7cm <em>with</em> large central MR jet (area < 40% of LA) or with a wall-impinging jet of any size, swirling in LA<sup>ψ</sup></li> | |||
<li>Large flow convergence<sup>ς</sup></li> | |||
<li>Systolic reversal in pulmonary veins</li> | |||
<li>Prominent flail MV leaflet or ruptured papillary muscle</li> | |||
</ul> | |||
|- | |||
! Supportive signs | |||
| style="vertical-align:top" | <ul> | |||
<li>Systolic dominant flow in pulmonary veins</li> | |||
<li>A-wave dominant mitral inflow<sup>Φ</sup></li> | |||
<li>Soft density, parabolic CW Doppler MR signal</li> | |||
<li>Normal LV size<sup>∗</sup></li> | |||
</ul> | |||
| style="vertical-align:top" colspan="2" | <ul><li>Intermediate signs/findings</li></ul> | |||
| style="vertical-align:top" | <ul> | |||
<li>Dense, triangular CW Doppler MR jet</li> | |||
<li>E-wave dominant mitral inflow (E >1.2 m/s)<sup>Φ</sup> Enlarged LV and LA size<sup>∗∗</sup>, (particularly when normal LV function is present).</li> | |||
</ul> | |||
|- | |||
| colspan="5" | '''Quantitative parameters<sup>φ</sup>''' | |||
|- | |||
| style="padding-left:12px" | R Vol (ml/beat) | |||
| align="center" | < 30 | |||
| style="width:125px" align="center" | 30-44 | |||
| style="width:125px" align="center" | 45-59 | |||
| align="center" | ≥ 60 | |||
|- | |||
| style="padding-left:12px" | RF (%) | |||
| align="center" | < 30 | |||
| align="center" | 30-39 | |||
| align="center" | 40-49 | |||
| align="center" | ≥ 50 | |||
|- | |||
| style="padding-left:12px" | EROA (cm<sup>2</sup>) | |||
| align="center" | < 0.20 | |||
| align="center" | 0.20-0.29 | |||
| align="center" | 0.30-0.39 | |||
| align="center" | ≥ 0.40 | |||
|- | |||
| colspan="5" | <ul> | |||
<li><em>CW</em>, Continuous wave; <em>EROA</em>, effective regurgitant orifice area; <em>LA</em>, left atrium; <em>LV</em>, left ventricle; <em>MV</em>, mitral valve; <em>MR</em>, mitral regurgitation; <em>R Vol</em>, regurgitant volume; <em>RF</em>, regurgitant fraction.</li> | |||
<li><sup>∗</sup> LV size applied only to chronic lesions. Normal 2D measurements: LV minor axis ≤ 2.8 cm/m<sup>2</sup>, LV end-diastolic volume ≤ 82 ml/m<sup>2</sup>, maximal LA antero-posterior diameter ≤ 2.8 cm/m<sup>2</sup>, maximal LA volume ≤ 36 ml/m<sup>2</sup> (2;33;35).</li> | |||
<li><sup>∗∗</sup> In the absence of other etiologies of LV and LA dilatation and acute MR.</li> | |||
<li><sup>ψ</sup> At a Nyquist limit of 50-60 cm/s.</li> | |||
<li><sup>Φ</sup> Usually above 50 years of age or in conditions of impaired relaxation, in the absence of mitral stenosis or other causes of elevated LA pressure.</li> | |||
<li><sup>ς</sup> Minimal and large flow convergence defined as a flow convergence radius < 0.4 cm and ≤ 0.9 cm for central jets, respectively, with a baseline shift at a Nyquist of 40 cm/s; Cut-offs for eccentric jets are higher, and should be angle corrected (see text).</li> | |||
<li><sup>φ</sup> Quantitative parameters can help sub-classify the moderate regurgitation group into mild-to-moderate and moderate-to-severe as shown.</li> | |||
</ul> | |||
|} | |||
==Mitral stenosis - severity== | |||
{| class="wikitable" style="font-size:90%;" | |||
|+'''Recommendations for classification of mitral stenosis severity<cite>ASEVS</cite>''' | |||
|- | |||
! style="width:200px" | | |||
! style="width:80px" | Mild | |||
! style="width:80px" | Moderate | |||
! style="width:80px" | Severe | |||
|- | |||
| colspan="4" | '''Specific findings''' | |||
|- | |||
| style="padding-left:12px" | Valve area (cm<sup>2</sup>) | |||
| align="center" | >1.5 | |||
| align="center" | 1.0-1.5 | |||
| align="center" | <1.0 | |||
|- | |||
| colspan="4" | '''Supportive findings''' | |||
|- | |||
| style="padding-left:12px" | Mean gradient (mmHg)<sup>a</sup> | |||
| align="center" | <5 | |||
| align="center" | 5-10 | |||
| align="center" | >10 | |||
|- | |||
| style="padding-left:12px" | Pulmonary artery pressure (mmHg) | |||
| align="center" | <30 | |||
| align="center" | 30-50 | |||
| align="center" | >50 | |||
|- | |||
| colspan="4" | <ul><li><sup>a</sup>At heart rates between 60 and 80 bpm and in sinus rhythm.</li></ul> | |||
|} | |||
==Mitral valve stenosis - Wilkins score== | ==Mitral valve stenosis - Wilkins score== | ||
{| class="wikitable" style="font-size:90%;" | {| class="wikitable" style="font-size:90%;" | ||
|+'''Assessment of mitral valve anatomy according to the Wilkins score< | |+'''Assessment of mitral valve anatomy according to the Wilkins score<cite>Wilkins</cite>''' | ||
|- | |- | ||
| Line 620: | Line 925: | ||
|} | |} | ||
==Mitral stenosis - routine measurements== | ==Mitral stenosis - routine measurements== | ||
{| class="wikitable" style="font-size:90%;" | {| class="wikitable" style="font-size:90%;" | ||
|+'''Recommendations for data recording and measurement in routine use for mitral stenosis quantitation''' | |+'''Recommendations for data recording and measurement in routine use for mitral stenosis quantitation<cite>ASEVS</cite>''' | ||
|- | |- | ||
| Line 632: | Line 936: | ||
|- | |- | ||
! Planimetry | ! rowspan="5" | Planimetry | ||
| | |||
|- | |||
| style="vertical-align:top; " | - 2D parasternal short-axis view | |||
| style="vertical-align:top; " | - contour of the inner mitral orifice | |||
|- | |||
| | | style="vertical-align:top; " | - determine the smallest orifice by scanning from apex to base | ||
| style="vertical-align:top; " | - include commissures when opened | |||
|- | |||
| style="vertical-align:top; " | - positioning of measurement plan can be oriented by 3D echo | |||
< | | style="vertical-align:top; " | - in mid-diastole (use cine-loop) | ||
|- | |||
| style="vertical-align:top" | - lowest gain setting to visualize the whole mitral orifice | |||
| style="vertical-align:top" | - average measurements if atrial fibrillation | |||
|- | |||
! rowspan="4" | Mitral flow | |||
|- | |||
| style="vertical-align:top; " | - continuous-wave Doppler | |||
| style="vertical-align:top; " | - mean gradient from the traced contour of the diastolic mitral flow | |||
|- | |||
| style="vertical-align:top; " | - apical windows often suitable (optimize intercept angle) | |||
| style="vertical-align:top; " | - pressure half-time from the descending sLope of the E-wave (mid-diastole slope if not linear) | |||
|- | |||
| style="vertical-align:top" | - adjust gain setting to obtain well-defined flow contour | |||
| style="vertical-align:top" | - average measurements if atrial fibrillation | |||
|- | |||
! rowspan="3" | Systolic pulmonary artery pressure | |||
|- | |||
| style="vertical-align:top; " | - continuous-wave Doppler | |||
| style="vertical-align:top; " | - maximum velocity of tricuspid regurgitant flow | |||
|- | |||
| style="vertical-align:top" | - multiple acoustic windows to optimize intercept angle | |||
| style="vertical-align:top" | - estimation of right atrial pressure according to inferior vena cava diameter | |||
|- | |||
! rowspan="8" | Valve anatomy | |||
|- | |||
| rowspan="2" style="vertical-align:top; " | | |||
- parasternal short-axis view | |||
|- | |||
| style="vertical-align:top; " | | |||
- valve thickness (maximum and heterogeneity)<br> | |||
- commissural fusion<br> | |||
- extension and location of localized bright zones (fibrous nodutes or calcification) | |||
|- | |- | ||
| rowspan="2" style="vertical-align:top; " | | |||
| | - parasternal long-axis view | ||
| | |||
|- | |- | ||
| style="vertical-align:top; " | | |||
- valve thickness<br> | |||
- extension of calcification<br> | |||
< | - valve pliability<br> | ||
- subvalvular apparatus (chordal thickening, fusion, or shortening) | |||
| | |- | ||
| rowspan="2" style="vertical-align:top" | - apical two-chamber view | |||
|- | |- | ||
| style="vertical-align:top; " | - subvalvular apparatus (chordal thickening, fusion, or shortening)<br> | |||
| | |- | ||
| colspan="2"| | |||
Detail each component and summarize in a score | |||
|} | |} | ||
== | |||
=Tricuspid Valve= | |||
==Tricuspid regurgitation - severity== | |||
{| class="wikitable" style="font-size:90%;" | {| class="wikitable" style="font-size:90%;" | ||
|+''' | |+'''Echocardiographic and Doppler parameters used in grading tricuspid regurgitation severity<cite>ASERE</cite>''' | ||
|- | |- | ||
! style="width:200px" | | ! style="width:200px" | Parameter | ||
! style="width: | ! style="width:200px" | Mild | ||
! style="width: | ! style="width:200px" | Moderate | ||
! style="width: | ! style="width:200px" | Severe | ||
|- | |||
| Tricuspid valve | |||
| Usually normal | |||
| Normal or abnormal | |||
| Abnormal/Flail leaflet/Poor coaptation | |||
|- | |- | ||
| | | RV/RA/IVC size | ||
| Normal<sup>∗</sup> | |||
| Normal or dilated | |||
| Usually dilated<sup>∗∗</sup> | |||
|- | |- | ||
| | | Jet area-central jets (cm<sup>2</sup>)<sup>§</sup> | ||
| < 5 | |||
| | | 5-10 | ||
| > 10 | |||
|- | |- | ||
| | | VC width (cm)<sup>Φ</sup> | ||
| Not defined | |||
| Not defined, but < 0.7 | |||
| > 0.7 | |||
|- | |- | ||
| | | PISA radius (cm)<sup>ψ</sup> | ||
| ≤ 0.5 | |||
| | | 0.6-0.9 | ||
| > 0.9 | |||
|- | |- | ||
| | | Jet density and contour–CW | ||
| | | Soft and parabolic | ||
| | | Dense, variable contour | ||
| | | Dense, triangular with early peaking | ||
|- | |- | ||
| | | Hepatic vein flow† | ||
| Systolic dominance | |||
| Systolic blunting | |||
| Systolic reversal | |||
|- | |||
| colspan="4" | | |||
<ul> | |||
<li><em>CW</em>, Continuous wave Doppler; <em>IVC</em>, inferior vena cava; <em>RA</em>, right atrium; <em>RV</em>, right ventricle; <em>VC</em>, vena contracta width.</li> | |||
<li><sup>∗</sup> Unless there are other reasons for RA or RV dilation. Normal 2D measurements from the apical 4-chamber view: RV medio-lateral end-diastolic dimension ≤ 4.3 cm, RV end-diastolic area ≤ 35.5 cm<sup>2</sup>, maximal RA medio-lateral and supero-inferior dimensions ≤ 4.6 cm and 4.9 cm respectively, maximal RA volume ≤ 33 ml/m<sup>2</sup>(35;89).</li> | |||
<li><sup>∗∗</sup> Exception: acute TR.</li> | |||
<li><sup>§</sup> At a Nyquist limit of 50-60 cm/s. Not valid in eccentric jets. Jet area is not recommended as the sole parameter of TR severity due to its dependence on | |||
hemodynamic and technical factors.</li> | |||
<li><sup>Φ</sup> At a Nyquist limit of 50-60 cm/s.</li> | |||
<li><sup>ψ</sup> Baseline shift with Nyquist limit of 28 cm/s.</li> | |||
<li>† Other conditions may cause systolic blunting (eg. atrial fibrillation, elevated RA pressure).</li> | |||
</ul> | |||
|} | |} | ||
==Tricuspid stenosis - severity== | ==Tricuspid stenosis - severity== | ||
{| class="wikitable" style="font-size:90%;" | {| class="wikitable" style="font-size:90%;" | ||
|+'''Findings indicative of haemodynamically significant tricuspid stenosis''' | |+'''Findings indicative of haemodynamically significant tricuspid stenosis<cite>ASEVS</cite>''' | ||
|- | |- | ||
| Line 752: | Line 1,105: | ||
|- | |- | ||
| style="padding-left:12px" | Valve area by continuity equation<sup>a</sup> | | style="padding-left:12px" | Valve area by continuity equation<sup>a</sup> | ||
| ≤1 cm<sup> | | ≤1 cm<sup>2</sup> | ||
|- | |- | ||
| Line 771: | Line 1,124: | ||
</ul> | </ul> | ||
|} | |} | ||
=Pulmonary Valve= | =Pulmonary Valve= | ||
==Pulmonary regurgitaion - severity== | |||
{| class="wikitable" style="font-size:90%;" | |||
|+'''Echocardiographic and Doppler parameters used in grading pulmonary regurgitation severity<cite>ASERE</cite>''' | |||
|- | |||
! style="width:200px" | Parameter | |||
! style="width:200px" | Mild | |||
! style="width:200px" | Moderate | |||
! style="width:200px" | Severe | |||
|- | |||
| Pulmonic valve | |||
| Normal | |||
| Normal or abnormal | |||
| Abnormal | |||
|- | |||
| RV size | |||
| Normal<sup>∗</sup> | |||
| Normal or dilated | |||
| Dilated | |||
|- | |||
| Jet size by color Doppler<sup>§</sup> | |||
| Thin (usually < 10 mm in length) with a narrow origin | |||
| Intermediate | |||
| Usually large, with a wide origin; May be brief in duration | |||
|- | |||
| Jet density and deceleration rate –CW† | |||
| Soft; Slow deceleration | |||
| Dense; variable deceleration | |||
| Dense; steep deceleration, early termination of diastolic flow | |||
|- | |||
| Pulmonic systolic flow compared to systemic flow –PW<sup>φ</sup> | |||
| Slightly increased | |||
| Intermediate | |||
| Greatly increased | |||
|- | |||
| colspan="4" | | |||
<ul> | |||
<li><em>CW</em>, Continuous wave Doppler; <em>PR</em>, pulmonic regurgitation; <em>PW</em>, pulsed wave Doppler; <em>RA</em>, right atrium; <em>RF</em>, regurgitant fraction; <em>RV</em>, right ventricle.</li> | |||
<li><sup>∗</sup> Unless there are other reasons for RV enlargement. Normal 2D measurements from the apical 4-chamber view; RV medio-lateral end-diastolic dimension ≤ 4.3 cm, RV end-diastolic area ≤ 35.5 cm<sup>2</sup>(89).</li> | |||
<li><sup>∗∗</sup> Exception: acute PR</li> | |||
<li><sup>§</sup> At a Nyquist limit of 50-60 cm/s.</li> | |||
<li><sup>φ</sup> Cut-off values for regurgitant volume and fraction are not well validated.</li> | |||
<li>† Steep deceleration is not specific for severe PR.</li> | |||
</ul> | |||
|} | |||
==Pulmonary stenosis - severity== | ==Pulmonary stenosis - severity== | ||
{| class="wikitable" style="font-size:90%;" | {| class="wikitable" style="font-size:90%;" | ||
|+'''Grading of pulmonary stenosis''' | |+'''Grading of pulmonary stenosis<cite>ASEVS</cite>''' | ||
|- | |- | ||
| Line 796: | Line 1,204: | ||
|} | |} | ||
=References= | =References= | ||
Click on the reference to link directly to the manuscript | |||
<biblio> | <biblio> | ||
#Foale pmid=3730205 | #Foale pmid=3730205 | ||
#Weyman isbn=0812112075 | #Weyman isbn=0812112075 | ||
#ASE pmid=16458610 | #ASE pmid=16458610 | ||
#ASEVS pmid=19130998 | |||
#Wilkins pmid=3190958 | |||
#ESCAS pmid=17259184 | |||
#ACCAS pmid=18848134 | |||
#ASERE pmid=12835667 | |||
#ASEDF pmid=19187853 | |||
#Hamer isbn=9031362352 | |||
</bilbio> | </bilbio> | ||
==External links== | |||
* [https://www.techmed.sk/en/echo/normal-values/ Normal echocardiography values - all measurements (TECHmED)] | |||
Latest revision as of 10:55, 19 March 2021
Below an up-to-date list of echocardiographic normal values.
Left Ventricle
Left Ventricular Systolic Function
| Women | Men | |||||||
|---|---|---|---|---|---|---|---|---|
| Reference range | Mildly abnormal | Moderately abnormal | Severely abnormal | Reference range | Mildly abnormal | Moderately abnormal | Severely abnormal | |
| Linear method | ||||||||
| Endocardial fractional shortening, % | 27–45 | 22–26 | 17–21 | ≤16 | 25–43 | 20–24 | 15–19 | ≤14 |
| Midwall fractional shortening, % | 15–23 | 13–14 | 11–12 | ≤10 | 14–22 | 12–13 | 10–11 | ≤10 |
| 2D Method | ||||||||
| Ejection fraction, % | ≥55 | 45–54 | 30–44 | <30 | ≥55 | 45–54 | 30–44 | <30 |
| ||||||||
Left Ventricular Diastolic Function
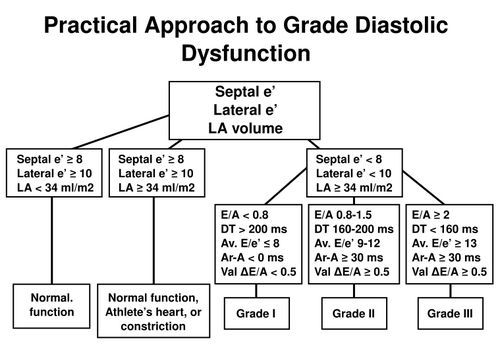
Practical approach to LV diastolic function grading. Ater [2]
| Age group (y) | ||||
|---|---|---|---|---|
| Measurement | 16-20 | 21-40 | 41-60 | >60 |
| IVRT (ms) | 50 ± 9 (32-68) | 67 ± 8 (51-83) | 74 ± 7 (60-88) | 87 ± 7 (73-101) |
| E/A ratio | 1.88 ± 0.45 (0.98-2.78) | 1.53 ± 0.40 (0.73-2.33) | 1.28 ± 0.25 (0.78-1.78) | 0.96 ± 0.18 (0.6-1.32) |
| DT (ms) | 142 ± 19 (104-180) | 166 ± 14 (138-194) | 181 ± 19 (143-219) | 200 ± 29 (142-258) |
| A duration (ms) | 113 ± 17 (79-147) | 127 ± 13 (101-153) | 133 ± 13 (107-159) | 138 ± 19 (100-176) |
| PV S/D ratio | 0.82 ± 0.18 (0.46-1.18) | 0.98 ± 0.32 (0.34-1.62) | 1.21 ± 0.2 (0.81-1.61) | 1.39 ± 0.47 (0.45-2.33) |
| PV Ar (cm/s) | 16 ± 10 (1-36) | 21 ± 8 (5-37) | 23 ± 3 (17-29) | 25 ± 9 (11-39) |
| PV Ar duration (ms) | 66 ± 39 (1-144) | 96 ± 33 (30-162) | 112 ± 15 (82-142) | 113 ± 30 (53-173) |
| Septal e´ (cm/s) | 14.9 ± 2.4 (10.1-19.7) | 15.5 ± 2.7 (10.1-20.9) | 12.2 ± 2.3 (7.6-16.8) | 10.4 ± 2.1 (6.2-14.6) |
| Septal e´/a´ ratio | 2.4∗ | 1.6 ± 0.5 (0.6-2.6) | 1.1 ± 0.3 (0.5-1.7) | 0.85 ± 0.2 (0.45-1.25) |
| Lateral e´ (cm/s) | 20.6 ± 3.8 (13-28.2) | 19.8 ± 2.9 (14-25.6) | 16.1 ± 2.3 (11.5-20.7) | 12.9 ± 3.5 (5.9-19.9) |
| Lateral e´/a´ ratio | 3.1∗ | 1.9 ± 0.6 (0.7-3.1) | 1.5 ± 0.5 (0.5-2.5) | 0.9 ± 0.4 (0.1-1.7) |
| ||||
Left Ventricular Mass and Geometry
| Women | Men | |||||||
|---|---|---|---|---|---|---|---|---|
| Reference range |
Mildly abnormal |
Moderately abnormal |
Severely abnormal |
Reference range |
Mildly abnormal |
Moderately abnormal |
Severely abnormal | |
| Linear Method | ||||||||
| LV mass, g | 67–162 | 163–186 | 187–210 | ≥211 | 88–224 | 225–258 | 259–292 | ≥293 |
| LV mass/BSA, g/m2 | 43–95 | 96–108 | 109–121 | ≥122 | 49–115 | 116–131 | 132–148 | ≥149 |
| LV mass/height, g/m | 41–99 | 100–115 | 116–128 | ≥129 | 52–126 | 127–144 | 145–162 | ≥163 |
| LV mass/height2, g/m2 | 18–44 | 45–51 | 52–58 | ≥59 | 20–48 | 49–55 | 56–63 | ≥64 |
| Relative wall thickness, cm | 0.22–0.42 | 0.43–0.47 | 0.48–0.52 | ≥0.53 | 0.24–0.42 | 0.43–0.46 | 0.47–0.51 | ≥0.52 |
| Septal thickness, cm | 0.6–0.9 | 1.0–1.2 | 1.3–1.5 | ≥1.6 | 0.6–1.0 | 1.1–1.3 | 1.4–1.6 | ≥1.7 |
| Posterior wall thickness, cm | 0.6–0.9 | 1.0–1.2 | 1.3–1.5 | ≥1.6 | 0.6–1.0 | 1.1–1.3 | 1.4–1.6 | ≥1.7 |
| 2D Method | ||||||||
| LV mass, g | 66–150 | 151–171 | 172–182 | >193 | 96–200 | 201–227 | 228–254 | >255 |
| LV mass/BSA, g/m2 | 44–88 | 89–100 | 101–112 | ≥113 | 50–102 | 103–116 | 117–130 | ≥131 |
| ||||||||
Left Ventricular Size
| Women | Men | |||||||
|---|---|---|---|---|---|---|---|---|
| Reference range |
Mildly abnormal |
Moderately abnormal |
Severely abnormal |
Reference range |
Mildly abnormal |
Moderately abnormal |
Severely abnormal | |
| LV dimension | ||||||||
| LV diastolic diameter | 3.9–5.3 | 5.4–5.7 | 5.8–6.1 | ≥6.2 | 4.2–5.9 | 6.0–6.3 | 6.4–6.8 | ≥6.9 |
| LV diastolic diameter/BSA, cm/m2 | 2.4–3.2 | 3.3–3.4 | 3.5–3.7 | ≥3.8 | 2.2–3.1 | 3.2–3.4 | 3.5–3.6 | ≥3.7 |
| LV diastolic diameter/height, cm/m | 2.5–3.2 | 3.3–3.4 | 3.5–3.6 | ≥3.7 | 2.4–3.3 | 3.4–3.5 | 3.6–3.7 | ≥3.8 |
| LV volume | ||||||||
| LV diastolic volume, mL | 56–104 | 105–117 | 118–130 | ≥131 | 67–155 | 156–178 | 179–201 | ≥201 |
| LV diastolic volume/BSA, mL/m2 | 35–75 | 76–86 | 87–96 | ≥97 | 35–75 | 76–86 | 87–96 | ≥97 |
| LV systolic volume, mL | 19–49 | 50–59 | 60–69 | ≥70 | 22–58 | 59–70 | 71–82 | ≥83 |
| LV systolic volume/BSA, mL/m2 | 12–30 | 31–36 | 37–42 | ≥43 | 12–30 | 31–36 | 37–42 | ≥43 |
| ||||||||
Right Ventricle
Right Ventricular and Pulmonary Artery Size
| Reference range | Mildly abnormal | Moderately abnormal | Severely abnormal | |
|---|---|---|---|---|
| RV dimensions | ||||
| Basal RV diameter (RVD 1), cm | 2.0–2.8 | 2.9–3.3 | 3.4–3.8 | ≥3.9 |
| Mid-RV diameter (RVD 2), cm | 2.7–3.3 | 3.4–3.7 | 3.8–4.1 | ≥4.2 |
| Base-to-apex length (RVD 3), cm | 7.1–7.9 | 8.0–8.5 | 8.6–9.1 | ≥9.2 |
| RVOT diameters | ||||
| Above aortic valve (RVOT 1), cm | 2.5–2.9 | 3.0–3.2 | 3.3–3.5 | ≥3.6 |
| Above pulmonic valve (RVOT 2), cm | 1.7–2.3 | 2.4–2.7 | 2.8–3.1 | ≥3.2 |
| PA diameter | ||||
| Below pulmonic valve (PA 1), cm | 1.5–2.1 | 2.2–2.5 | 2.6–2.9 | ≥3.0 |
| ||||
Right Ventricular Size and Function
| Reference range | Mildly abnormal | Moderately abnormal | Severely abnormal | ||
|---|---|---|---|---|---|
| RV diastolic area, cm2 | 11–28 | 29–32 | 33–37 | ≥38 | |
| RV systolic area, cm2 | 7.5–16 | 17–19 | 20–22 | ≥23 | |
| RV fractional area change, % | 32–60 | 25–31 | 18–24 | ≤17 | |
| TAPSE, (cm) | 1.5-2.0[1] | 1.3-1.5[4] | 1.0-1.2[4] | <1.0[4] | |
| |||||
Atria
Left Atrial Dimensions / Volumes
| Women | Men | |||||||
|---|---|---|---|---|---|---|---|---|
| Reference range | Mildly abnormal | Moderately abnormal | Severely abnormal | Reference range | Mildly abnormal | Moderately abnormal | Severely abnormal | |
| Atrial dimensions
| ||||||||
| LA diameter, cm | 2.7–3.8 | 3.9–4.2 | 4.3–4.6 | ≥4.7 | 3.0–4.0 | 4.1–4.6 | 4.7–5.2 | ≥5.2 |
| LA diameter/BSA, cm/m2 | 1.5–2.3 | 2.4–2.6 | 2.7–2.9 | ≥3.0 | 1.5–2.3 | 2.4–2.6 | 2.7–2.9 | ≥3.0 |
| RA minor-axis dimension, cm | 2.9–4.5 | 4.6–4.9 | 5.0–5.4 | ≥5.5 | 2.9–4.5 | 4.6–4.9 | 5.0–5.4 | ≥5.5 |
| RA minor-axis dimension/BSA, cm/m2 | 1.7–2.5 | 2.6–2.8 | 2.9–3.1 | ≥3.2 | 1.7–2.5 | 2.6–2.8 | 2.9–3.1 | ≥3.2 |
| Atrial area | ||||||||
| LA area, cm2 | ≤20 | 20–30 | 30–40 | >40 | ≤20 | 20–30 | 30–40 | >40 |
| Atrial volumes | ||||||||
| LA volume, mL | 22–52 | 53–62 | 63–72 | ≥73 | 18–58 | 59–68 | 69–78 | ≥79 |
| LA volume/BSA, mL/m2 | 22 ± 6 | 29–33 | 34–39 | ≥40 | 22 ± 6 | 29–33 | 34–39 | ≥40 |
| ||||||||
Left Atrial Pressure
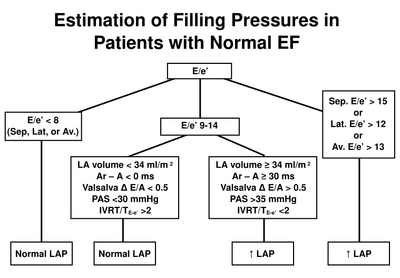
Estimation of left atrial pressure in normal LVEF. After [2]
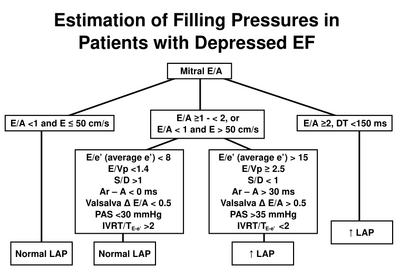
Estimation of left atrial pressure in reduced LVEF. After [2]
Aortic Valve
Aortic valve stenosis - severity
| Aortic sclerosis | Mild | Moderate | Severe | |
|---|---|---|---|---|
| Aortic jet velocity (m/s) | ≤2.5 m/s | 2.6-2.9 | 3.0-4.0 | >4.0 |
| Mean gradient (mmHg) | - | <20 (<30a) | 20-40b (30-50a) | >40b (>50a) |
| AVA (cm2) | - | >1.5 | 1.0-1.5 | <1 |
| Indexed AVA (cm2/m2) | >0.85 | 0.60-0.85 | <0.6 | |
| Velocity ratio | >0.50 | 0.25-0.50 | <0.25 | |
Aortic regurgitation - severity
| Mild | Moderate | Severe | ||
|---|---|---|---|---|
| Specific signs for AR severity |
|
|
| |
| Supportive signs |
|
|
| |
| Quantitative parametersψ | ||||
| R Vol, ml/beat | < 30 | 30-44 | 45-59 | ≥ 60 |
| RF % | < 30 | 30-39 | 40-49 | ≥ 50 |
| EROA, cm2 | < 0.10 | 0.10-0.19 | 0.20-0.29 | ≥ 0.30 |
| ||||
Mitral Valve
Mitral regurgitation - severity
| Mild | Moderate | Severe | ||
|---|---|---|---|---|
| Specific signs of severity |
|
|
| |
| Supportive signs |
|
|
| |
| Quantitative parametersφ | ||||
| R Vol (ml/beat) | < 30 | 30-44 | 45-59 | ≥ 60 |
| RF (%) | < 30 | 30-39 | 40-49 | ≥ 50 |
| EROA (cm2) | < 0.20 | 0.20-0.29 | 0.30-0.39 | ≥ 0.40 |
| ||||
Mitral stenosis - severity
| Mild | Moderate | Severe | |
|---|---|---|---|
| Specific findings | |||
| Valve area (cm2) | >1.5 | 1.0-1.5 | <1.0 |
| Supportive findings | |||
| Mean gradient (mmHg)a | <5 | 5-10 | >10 |
| Pulmonary artery pressure (mmHg) | <30 | 30-50 | >50 |
| |||
Mitral valve stenosis - Wilkins score
| Grade | Mobility | Thickening | Calcification | Subvalvular Thickening |
|---|---|---|---|---|
| 1 | Highly mobile valve with only leaflet tips restricted | Leaflets near normal in thickness (4-5 mm) | A single area of increased echo brightness | Minimal thickening just below the mitral leaflets |
| 2 | Leaflet mid and base portions have normal mobility | Midleaflets normal, considerable thickening of margins (5-8 mm) | Scattered areas of brightness confined to leaflet margins | Thickening of chordal structures extending to one-third of the chordal length |
| 3 | Valve continues to move forward in diastole, mainly from the base | Thickening extending through the entire leaflet (5-8mm) | Brightness extending into the mid-portions of the leaflets | Thickening extended to distal third of the chords |
| 4 | No or minimal forward movement of the leaflets in diastole | Considerable thickening of all leaflet tissue (>8-10mm) | Extensive brightness throughout much of the leaflet tissue | Extensive thickening and shortening of all chordal structures extending down to the papillary muscles |
| ||||
Mitral stenosis - routine measurements
| Data element | Recording | Measurement |
|---|---|---|
| Planimetry | ||
| - 2D parasternal short-axis view | - contour of the inner mitral orifice | |
| - determine the smallest orifice by scanning from apex to base | - include commissures when opened | |
| - positioning of measurement plan can be oriented by 3D echo | - in mid-diastole (use cine-loop) | |
| - lowest gain setting to visualize the whole mitral orifice | - average measurements if atrial fibrillation | |
| Mitral flow | ||
| - continuous-wave Doppler | - mean gradient from the traced contour of the diastolic mitral flow | |
| - apical windows often suitable (optimize intercept angle) | - pressure half-time from the descending sLope of the E-wave (mid-diastole slope if not linear) | |
| - adjust gain setting to obtain well-defined flow contour | - average measurements if atrial fibrillation | |
| Systolic pulmonary artery pressure | ||
| - continuous-wave Doppler | - maximum velocity of tricuspid regurgitant flow | |
| - multiple acoustic windows to optimize intercept angle | - estimation of right atrial pressure according to inferior vena cava diameter | |
| Valve anatomy | ||
|
- parasternal short-axis view | ||
|
- valve thickness (maximum and heterogeneity) | ||
|
- parasternal long-axis view | ||
|
- valve thickness | ||
| - apical two-chamber view | ||
| - subvalvular apparatus (chordal thickening, fusion, or shortening) | ||
|
Detail each component and summarize in a score | ||
Tricuspid Valve
Tricuspid regurgitation - severity
| Parameter | Mild | Moderate | Severe |
|---|---|---|---|
| Tricuspid valve | Usually normal | Normal or abnormal | Abnormal/Flail leaflet/Poor coaptation |
| RV/RA/IVC size | Normal∗ | Normal or dilated | Usually dilated∗∗ |
| Jet area-central jets (cm2)§ | < 5 | 5-10 | > 10 |
| VC width (cm)Φ | Not defined | Not defined, but < 0.7 | > 0.7 |
| PISA radius (cm)ψ | ≤ 0.5 | 0.6-0.9 | > 0.9 |
| Jet density and contour–CW | Soft and parabolic | Dense, variable contour | Dense, triangular with early peaking |
| Hepatic vein flow† | Systolic dominance | Systolic blunting | Systolic reversal |
| |||
Tricuspid stenosis - severity
| Specific findings | |
| Mean pressure gradient | ≥5 mmHg |
| Inflow time-velocity integral | >60 cm |
| T1/2 | ≥190 ms |
| Valve area by continuity equationa | ≤1 cm2 |
| Supportive findings | |
| Enlarged right atrium ≥moderate | |
| DHated inferior vena cava | |
| |
Pulmonary Valve
Pulmonary regurgitaion - severity
| Parameter | Mild | Moderate | Severe |
|---|---|---|---|
| Pulmonic valve | Normal | Normal or abnormal | Abnormal |
| RV size | Normal∗ | Normal or dilated | Dilated |
| Jet size by color Doppler§ | Thin (usually < 10 mm in length) with a narrow origin | Intermediate | Usually large, with a wide origin; May be brief in duration |
| Jet density and deceleration rate –CW† | Soft; Slow deceleration | Dense; variable deceleration | Dense; steep deceleration, early termination of diastolic flow |
| Pulmonic systolic flow compared to systemic flow –PWφ | Slightly increased | Intermediate | Greatly increased |
| |||
Pulmonary stenosis - severity
| Mild | Moderate | Severe | |
|---|---|---|---|
| Peak velocity (m/s) | <3 | 3-4 | >4 |
| Peak gradient (mmHg) | <36 | 36-64 | >64 |
References
Click on the reference to link directly to the manuscript <biblio>
- Foale pmid=3730205
- Weyman isbn=0812112075
- ASE pmid=16458610
- ASEVS pmid=19130998
- Wilkins pmid=3190958
- ESCAS pmid=17259184
- ACCAS pmid=18848134
- ASERE pmid=12835667
- ASEDF pmid=19187853
- Hamer isbn=9031362352
</bilbio>