Aorta: Difference between revisions
(Created page with "==Aortic Dimensions== {| class="wikitable" cellpadding="0" cellspacing="0" border="0" width="800px" |- !colspan="2"|Aortic diameters (BSAindex) |- |Aortic annulus |20 - 31mm...") |
(No difference)
|
Revision as of 22:22, 4 January 2014
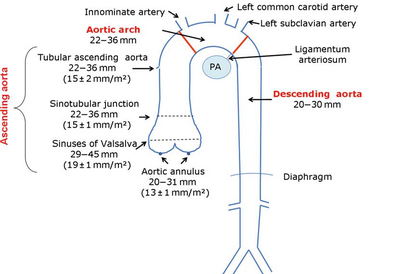
Aortic Dimensions
| Aortic diameters (BSAindex) | |
|---|---|
| Aortic annulus | 20 - 31mm (13 ± 1mm/m2) |
| Aortic Root | 29 - 45mm (19 ± 1mm/m2) |
| Sinotubular junction | 22 - 36mm (15 ± 1mm/m2) |
| Tube | 22 - 36mm (15 ± 2mm/m2) |
| Aortic Arch | 22 -36mm |
| Descending aorta | 20 -30mm |
| Abdominal aorta | 20 -30mm |
| NB. In contrast to tomographic methods, the echocardiographic derived measures are reported as internal diameters. "Recommendations for Aortic Imaging Techniques to Determine the Presence and Progression of Thoracic Aortic Disease".1 | |
|
| Picture source: European Journal of Echocardiography (2010 ) 11 , 645-6582 |
|---|
Aortic dissection
Diagnostic is an undulating motion intimal flap , which in more recordings and directions must be seen. The flap should have a movement that is not parallel with any other cardio -thoracic structure .
Upon dissection mind : - Location of dissection - Type A ( involvement of ascending aorta ) - Type B ( no involvement of ascending aorta ) - Location of intimal tear - Location of re-entry and possibly tear . another crack - Involvement of aortic arch and outgoing vessels - Differentiation between true and false lumen - Involvement of coronary arteries - The presence of aortic valve insufficiency - Pericardium moisture - LV function It also shows the intramural hematoma of the aorta to be aware of the aortic dissection. One variant This does not intraluminal flap was observed making the diagnosis is difficult to establish . Echocardiographic is viewed as a thickened aortic wall .
Differentiation between true and false lumen:- In M mode, the flap moves to the false lumen in systole. - Spontaneous echo contrast and thrombus can be seen in the false lumen . - With color Doppler is delayed systolic flow seen by secondary or re-entry tear to the false lumen. - The false lumen (especially in chronic dissections) tends to be larger in comparison to the true lumen. aortic coarctation Imaging of the aortic arch usually works best from the jugular (sternal supra). When evaluating a patient with a suspected coarctation always pay attention to associated anomalies such as: - Bicuspid aortic valve - Aortic valve stenosis - Patent ductus arteriosus - VSD - Mitral valve abnormalities
Determining coarctation Note instrument Location Color doppler The origo of the carotid and subclavian artery are reference points for locating the coarctation.
Continuous wave velocity profile Remember that collaterals systolic maximum speed but does reduce the diastolic gradient persists . In the presence of diastolic forward flow refers to a hemodynamically significant coarctation . Typical CW Doppler signal from descending aorta with diastolic forward flow matching hemodynamically significant coarctation.2
References
<biblio>
- 1 pmid=20233780
- 2 pmid=20823280
</biblio>