Right Ventricle: Difference between revisions
No edit summary |
|||
| Line 111: | Line 111: | ||
{| class="wikitable" cellpadding="0" cellspacing="0" border="0" | {| class="wikitable" cellpadding="0" cellspacing="0" border="0" | ||
|- | |- | ||
![[Image:RVFAC01.png| | ![[Image:RVFAC01.png|350px]] | ||
Good RV function | Good RV function | ||
![[Image:RVFAC02.png| | ![[Image:RVFAC02.png|350px]] | ||
Decreased RV function | Decreased RV function | ||
Revision as of 14:50, 18 November 2013
The Right Ventricle
The contractile function of the RV is difficult to measure due to the complex anatomy. Historically in clinical practice there was very little attention paid to this part of the heart, since it was assumed that they previously played a passive role. Only in the last three decades it has been shown that the function of the RV plays an important role in the survival of several disease states. There is also a number of echocardiographic measurements to measure RV function and provide insight into the mechanisms of RV dysfunction.
Right ventricular dimensions
| Reference range | Mildly abnormal | Moderately abnormal | Severely abnormal | |
|---|---|---|---|---|
| RV dimensions | ||||
| Basal RV diameter (RVD 1), cm | 2.0–2.8 | 2.9–3.3 | 3.4–3.8 | ≥3.9 |
| Mid-RV diameter (RVD 2), cm | 2.7–3.3 | 3.4–3.7 | 3.8–4.1 | ≥4.2 |
| Base-to-apex length (RVD 3), cm | 7.1–7.9 | 8.0–8.5 | 8.6–9.1 | ≥9.2 |
| *RV diastolic area, cm2 | 11–28 | 29–32 | 33–37 | ≥38 |
| *RV systolic area, cm2 | 7.5–16 | 17–19 | 20–22 | ≥23 |
| RVOT diameters | ||||
| Above aortic valve (RVOT 1), cm | 2.5–2.9 | 3.0–3.2 | 3.3–3.5 | ≥3.6 |
| Above pulmonic valve (RVOT 2), cm | 1.7–2.3 | 2.4–2.7 | 2.8–3.1 | ≥3.2 |
| *Reference limits and partition values of right ventricular size and function as measured in apical 4-chamber view. | ||||
Right ventricular function
| Reference range | Mildly abnormal | Moderately abnormal | Severely abnormal | |
|---|---|---|---|---|
| *RV fractional area change, % | 32–60 | 25–31 | 18–24 | ≤17 |
| *TAPSE, cm | 1.5-2.0 | 1.3-1.5 | 1.0-1.2 | <1.0 |
| *RV MPI | <0.28 | |||
| *Dp/DT | >400mmHg | |||
| *RV TDI doppler (S'), cm/s | >11.5 | |||
| *Reference limits and partition values of right ventricular size and function as measured in apical 4-chamber view.1 | ||||
Fractional Area Change
With this method, the percentage difference in the surface traced by the RV measured during systole and diastole is measured. Here again the apical 4CH is used for accuracy. The difference in surface limited to less than 35%, then this fits a reduced function. This method is frequently used in clinical practice.
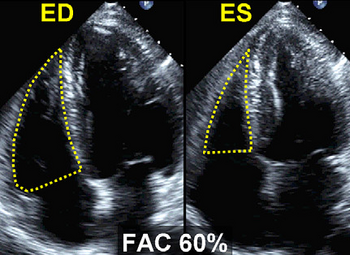
Good RV function |
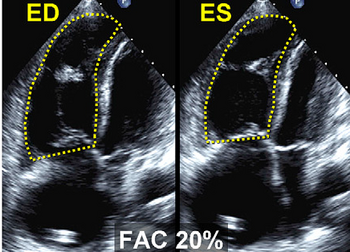
Decreased RV function |
|---|
Dp/DT
These methods make use of determining the speed of the myocardium itself and determination of pressure differences between the compartments of the right heart. A simple physiological measure of RV function is the systolic pressure buildup in the time of the RV. This can be determined as Dp/DT, for this purpose, the systolic acceleration speed of the tricuspid insufficiency signal is determined during the isovolumetric contraction phase. This can be done by measuring the time interval in the continuous wave signal TR is between 1 and 2m/s.
Due to that, by definition, a differential pressure of 12mmHg is concerned, this size will be determined by dividing by 12, the measured time interval. Quite simply the pressure build-up is less than 400mmHg/sec then this is an indication for a reduced right ventricular function.
Click here for dP/DT calculation.
RV myocardial performance index (MPI)
The MPI or Tei index is a dimensionless index and a measure of efficiency of the systole. This index is the ratio between the sum of both isovolumic times and ejection. The isovolumic relaxation time is the time between the closing of the pulmonary valve and the beginning of the opening of the tricuspid valve. The time in which blood flows through the pulmonary valve is called the EJECT time. The larger the portion of the time that is used for actual ejection of blood, the better the function of the room. This is the underlying idea of the performance index. So the higher the index, the less efficient the RV .
Unfortunately, it is often difficult to measure. The isovolumic contraction and relaxation phases exactly It does not have too.
What you can use is the time between the conclusion of the TV and access the back of the TV ( tricuspid closing to opening time). This can be determined by measuring between the end of the A-wave and the beginning of the next E-top on the TV influx signal on the recording AP4CH the duration.
If you are also in the measurement of RV ejection in Plax shot, here you can quickly and easily determine the total duration of the isovolumic times. This is because the difference between the TV closing to opening time and the EJECT time. Share time again by the EJECT time and you have the MPI.
The normal values of left and right ventricular differences. Due to the high pressures which must generate the LV, the isovolumetric times of the LV relatively long. The RV has it in the normal situation easier, and therefore the index also lower average at around 0:28.
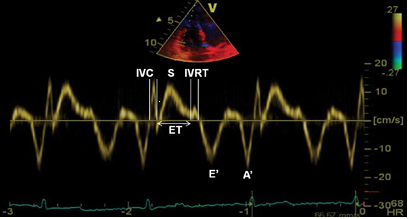
RV MPI measured using TDI and PW in TVannulus. |
|---|
Click here for MPI calculation.
The determination of the RV function, occurs regularly on the eye, or even not at all. Unfortunately, this ensures that many RV pathology is not recognized. Using various echo techniques can be a good statement about the function of the RV done. Never use a technique, but always more. This reduces the risk of troublesome and even erroneous interpretations.2
References
<biblio>
- 1 pmid=20620859
- 2 pmid=15842967
</biblio>